BACKGROUND: Advances in novel therapies and supportive care have contributed to improved outcomes for patients with Multiple myeloma (MM) and Light Chain Amyloidosis (AL). This progress comes at a high price; with high financial costs to patients increasing distress, decreasing compliance, and even decreasing survival. Our aim was to screen patients for financial distress and understand its impact on various domains of health-related quality of life (HRQOL).
METHODS: We conducted a prospective study of adult patients with MM or AL that received follow-up care at Mayo Clinic, Rochester, MN. Financial distress was measured using the validated COmprehensive Score for financial Toxicity (COST) questionnaire; high financial distress was defined as a score of 23 or less. HRQOL was measured using the Patient Reported Outcome Measurement Information System (PROMIS)-29 questionnaire. Baseline demographic information and clinical characteristics were abstracted from the medical record. Statistical analysis included descriptive statistics, Spearman correlations, and comparison of COST scores between groups by Jonckheere-Terpstra, Kruskal-Wallis, and Wilcoxon rank-sum tests for ordered, unordered, and binary categorical variables, respectively.
RESULTS: Patients: To date 77 patients (MM 64 [83%], AL 13 [17%]) have been enrolled, 55% male, 53% age 65 or older (18% <55), 91% White (5% Black), 92% non-Hispanic, 56% at least some college, 47% income at least US$75K/year (25% <US 50K/year), 36% employed (49% retired), 73% married (14% divorced) and 22% traveled at least 300 miles to clinic. Clinical characteristics included 45% newly diagnosed, 55% relapsed/refractory disease. 66% had been transplanted previously. Insurance types included 52% Medicare (44% private insurance) with 27% overall reporting supplemental insurance.
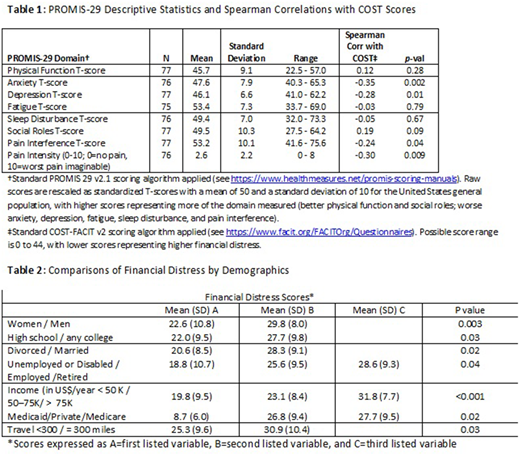
Financial Distress: The mean COST score was 26.5 (SD 10.0) with 42% reporting high financial distress. PROMIS-29 domain descriptive statistics appear in Table 1. Higher financial distress was significantly associated with higher anxiety, depression, and pain (all p<0.05).
Group Differences: Financial distress significantly differed by gender, education, marital status, employment status, income, insurance type, and distance traveled reported in Table 2. Financial distress was higher: in women than men (p=0.003); in high school graduates vs those who attended some college or more (p=0.03); in divorced versus married individuals (p=0.02); among unemployed or disabled versus employed versus retired people (p=0.04); in those with income <US$50K/year versus US$50K-<$75K/year versus at least US$75K/year (p<0.001); among those with Medicaid vs private insurance versus Medicare (p=0.02); and for those whose distance from Mayo was at least 300 miles vs < 300 miles (p=0.03). Differences in age neared but failed to reach strict statistical significance (age 35-54: mean 22.4, SD 12.1; age 55-64: mean 26.5, SD 9.5; age 65+: mean 28.0, SD 9.2; p=0.051). Financial distress did not significantly differ by race, ethnicity, diagnosis, disease status (newly diagnosed/relapsed), prior transplant, or supplemental insurance, though some subgroups were small.
CONCLUSION: Financial distress was prevalent in this well-educated and high earning MM and AL cohort that is able to receive tertiary care at Mayo Clinic. This financial distress was moderate to strongly associated with anxiety and pain intensity, and mild to moderately associated with depression and pain interference. Longitudinal assessment is ongoing.
Dispenzieri:Takeda: Research Funding; Celgene: Research Funding; Janssen: Research Funding; Pfizer: Research Funding; Alnylam: Research Funding; Intellia: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal